A Trusted Solution for Complex Discharges: Safehaven Offers Stability for Patients with Brain Injuries and Ventilator Dependency
Exploring Safehaven's unique, home-like environment tailored for brain-injured and ventilator-dependent patients, discussing key considerations for discharge, compliance, and evidence of how our services can enhance patient outcomes.

Did you know that transitioning patients with brain injuries or those who are ventilator-dependent from hospital to long-term care can be challenging for healthcare professionals? This blog post provides valuable insights for discharge planners, case managers, and healthcare providers on how to successfully navigate these complexities. We will explore Safehaven's unique, home-like environment tailored for brain-injured and ventilator-dependent patients, discussing key considerations for discharge, compliance, and evidence of how our services can enhance patient outcomes.
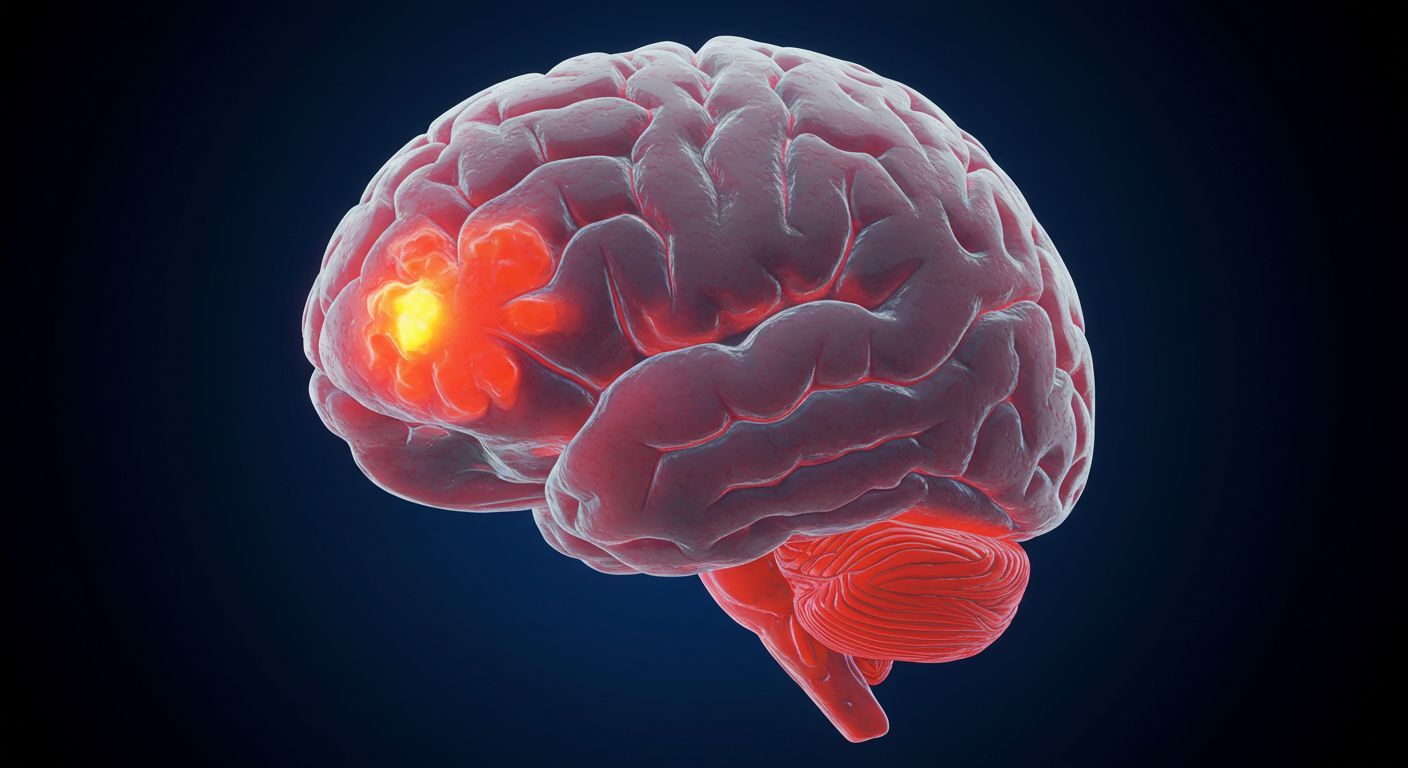
Understanding Brain Injuries and Ventilator Dependency
Brain injuries can arise from various causes, including trauma, infections, lack of oxygen, or strokes. These injuries can manifest with diverse symptoms and impairments which complicate recovery and care. Recognizing the unique challenges goes beyond understanding the physical implications; patients may also face cognitive and emotional challenges. Similarly, ventilator-dependent patients require ongoing respiratory support, making discharge planning pivotal for their continued health.
Challenges of Discharging Patients with Brain Injuries and Ventilator Dependency
Discharge planners and healthcare providers encounter several significant challenges when caring for these patients:
- Complex Care Needs: Both brain-injured and ventilator-dependent patients require specialized medical care that many facilities may not be equipped to provide.
- Safety and Compliance: Finding a care environment that adheres to clinical guidelines while ensuring the patient's safety can be daunting.
- Family Involvement: Family members need to be actively engaged in the discharge process, yet they often struggle with understanding the complexities of post-hospitalization care.
- Continuity of Care: Any misstep in the transition can lead to lapses in care, affecting the patient’s recovery journey.
Safehaven: A Thoughtful Solution for Complex Discharges
At Safehaven, we are committed to overcoming these challenges and offering an approach that emphasizes quality care tailored to individual needs. Here are some of our key services:
- 24/7 Skilled Nursing Care: Our healthcare professionals provide continuous medical oversight, ensuring that patients receive individualized attention on all fronts. This continuous monitoring can prove essential in responding to sudden changes in health status.
- Specialized Care for Brain Injuries: Every patient at Safehaven benefits from personalized rehabilitation plans tailored to their specific needs, whether cognitive therapy or physical rehabilitation, promoting a smooth recovery process.
- Comprehensive Ventilator Support: Our team is equipped to address the complexities involved with ventilator care, adapting to changes in the patient’s health so that necessary interventions can be made promptly.
- Engaging Activities and Support: Emotional and psychological well-being is addressed through organized activities that remember each patient’s unique needs, fostering a sense of community.
- Family Support and Respite Care: Family caregivers often face emotional and physical fatigue. We provide educational resources and support to ensure families are informed and acknowledged throughout this process.
Ensuring Compliance and Positive Outcomes
A major benefit of Safehaven stems from our unwavering commitment to compliance with all applicable guidelines and standards. Every aspect of our care model is designed to provide peace of mind for both healthcare providers and families:
- Patient Outcomes: Evidence increasingly shows that patients with brain injuries or those who are ventilator-dependent experience better health results when transitioned to a supportive long-term care facility. Safehaven patients often enjoy improved health metrics and a reduced need for hospitalization thereafter.
Engaging Healthcare Professionals: Navigating Discharge Planning
Providers and discharge planners can significantly enhance care transitions by following intentional steps:
- Integrate Early Communication: Consult with Safehaven’s team during the initial stages of discharge planning to gather essential insights and streamline transitions.
- Foster Open Dialogue: Create an ongoing dialogue with the care team at Safehaven to facilitate patient status updates and necessary adjustments in the care plan.
- Empower Families: Equip family members with relevant information about upcoming changes, addressing any concerns and fostering trust in the care environment.
- Solicit Feedback: Construct feedback mechanisms to learn from patients and families about their transition experience, creating an opportunity for ongoing improvement in processes.
The Path Forward for Patients with Brain Injuries and Ventilator Dependency
Transitioning these patients from hospital care to a sustainable long-term facility can be daunting, but Safehaven is here to support every step of the way. Our commitment to quality, safety, and compassionate care underscores the decisions made by case managers and healthcare providers in their patient placements.
Effective transitioning not only aids in enhancing recovery but also improves the trust placed in healthcare systems by families. By initiating early interventions and fostering ongoing communication, smoother transitions can be secured. Whether you are looking to refer a patient, schedule a call with our team, download our referral guide, or request bed availability, collaborating with Safehaven fosters hope, security, and dignity for patients and their families alike.
Request Bed Availability and let us assist you in this vital process. We believe that empathy and professionalism go hand in hand, shaping a brighter future for those we care for.